Hydrops (or corneal rupture) is a rare complication of severe keratoconus eye disease. So much so, that at The Eye Practice, we only see three or four cases a year.
‘Hydrops’ is the term used to describe an accumulation of fluid somewhere in the body. In corneal hydrops, a sudden tear in one of the corneal membranes allows fluid from inside the eye to leak into your corneal tissue.
But is this a disaster for keratoconus sufferers?
What happens to the cornea during hydrops?
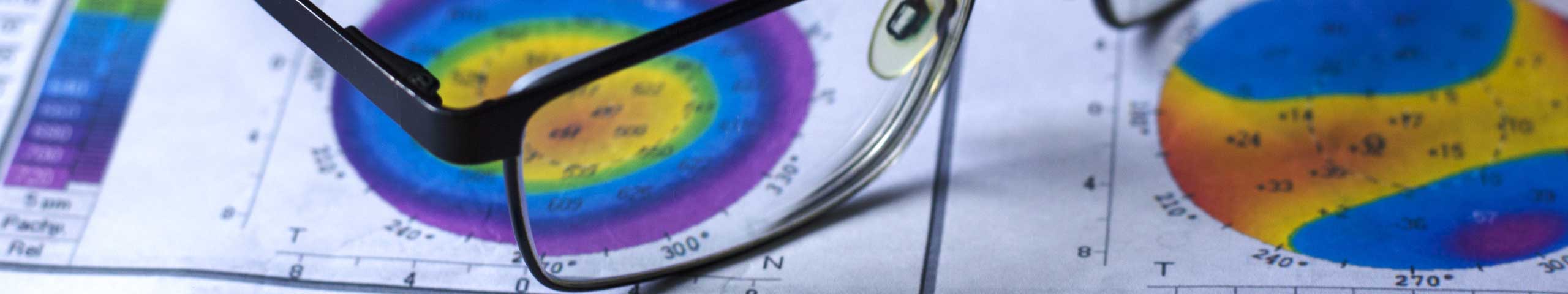
Your cornea is composed of layers, with a thick central layer (the stroma) sandwiched between thinner layers and membranes on each side. The inner-most membrane is called Descemet’s membrane and is strong and elastic. It acts a barrier to fluid from inside the eye leaking into the cornea.
When corneal hydrops occurs in keratocous, Descement’s membrane ruptures, allowing fluid to seep into the cornea. This alters the transparency of the cornea, so you see a milky appearance in the affected area. This event is usually accompanied by pain, swelling and a marked deterioration in vision.
Does it hurt?
This condition is acute (or sudden) in onset, and is usually accompanied by pain and a scratchy sensation in the eye. You should see your keratoconus practitioner as soon as possible. They will carefully examine your eyes, prescribe eye drops to reduce the pain and discomfort and may refer you to a corneal specialist in severe cases.
How will I know if I have hydrops?
This is a rare condition, so if you suddenly develop a painful, red eye with poor vision, it may be that you don’t have hydrops at all, but have a corneal infection related to your contact lens wear. An infection in your cornea is a serious and sight-threatening condition which requires prompt treatment.
Only an experienced practitioner can diagnose hydrops on examination of your eyes. Either way, if your eye suddenly becomes red, irritated, watery and much more blurred, you need to see your practitioner urgently.
Is it permanent?
No! In most cases, this is a temporary effect and milkiness clears over a couple of months. You may be given anti-inflammatory (and other) eyedrops to help with pain and swelling and to allow the cornea to clear up more quickly.
You will be left with a scar at the site of the original tear in the membrane, but this is often offset from the centre of your vision and often causes little deterioration.
What causes hydrops?
This condition occurs spontaneously in people who have advanced or severe keratoconus.
Will I need a graft?
Corneal transplantation is not usually indicated during corneal hydrops. Once the milkiness clears (after a month or two) you will be left with a scar at the site of the original membrane tear. But this scar is not usually central and doesn’t mean your vision will be impacted.
If the scar is more central and impacting on your vision significantly, a corneal transplant may be required.
The silver lining?
Sometimes, corneal hydrops will actually have some upside. It often creates a flatter corneal profile, once the cornea has settled down, making it easier to fit contact lenses successfully.
Once the cornea has cleared, you will be left with a scar at the site of the tear. As long as it’s not central, this can actually work to make your cornea stronger.