Meibomian gland dysfunction (MGD) is a common, chronic abnormality of the meibomian glands. This results in the glands becoming blocked and the oil they produce becoming thickened and reduced in quality. It is one of the most common eye conditions.
MGD leads to evaporative dry eye – where the watery tear layer has no protection from evaporating. Evaporative dry eye is the leading cause of dry eye disease (1). This causes symptoms of dry, irritated eyes. It almost always affects both eyes, but it may be worse in one eye than the other. Dry eye is a very common condition that can cause a variety of signs and symptoms which have a significant interference on quality of life.
People with early MGD may not experience any symptoms at all. The condition is progressive in nature, however, and patients are likely to become more and more symptomatic as the glands become more obstructed over time.
What do the meibomian glands do?
Meibomian glands are special oil glands in the upper and lower eyelids. There are approximately 50 glands in the upper eyelids and 25 glands in the lower eyelids. The glands produce an oil which is a very important part of our tears. Our tears comprise three layers or components: the lipid (oil) layer, aqueous (water) layer, and the mucous (sticky) layer. The three layers work in unison to lubricate the eye. The function of the oil produced by the meibomian glands is to stop (or reduce) evaporation of the watery tears from the surface of our eyes. This keeps our eyes feeling comfortable and lubricated.
Symptoms
Symptoms of MGD include: Crusty or sticky or eyelids, especially near the base of the eyelashes; Dryness (MGD is implicated in 70% of all dry eyes); Red, sore, gritty eyes; Difficulty with contact lens wear, leading to failure to successfully wear your lenses; Watery eyes.
Often, people with MGD start to use eye drops from the pharmacy to make their eyes feel lubricated. Unfortunately most of these drops only work for a very short period of time, because without an adequate layer of Meibomian Gland oil, the drops simply evaporate off the eye
Oddly, sometimes the eyes can become watery. This is because the watery layer of tears is normal, however there is not adequate oil to keep the tears on the surface of the eye. Also, the eye irritation may produce increased watery tears as a reflex action – but again, the tears are unable to stay on the eyes for long enough to keep them lubricated.
Causes of MGD
Meibomian gland dysfunction occurs when the oil-producing glands in the eyelids are impaired. This may be due to:
Skin conditions
Such as acne rosacea is commonly seen with MGD
Some medications
Such as Roaccutane for acne, can alter the MG secretions and cause them to become blocked
Blepharitis
The World’s most common eye disease. It results from a biofilm of bacteria colonising the skin of the eyelid margins. Exotoxins from these bacteria can enter the meibomian glands and cause a reduction in quality or quantity of tears.
Altered levels fatty acids
Altered levels of Omega-3 and -6 fatty acids in the body are common with the modern western diet. This can lead to impaired function of the oil glands.
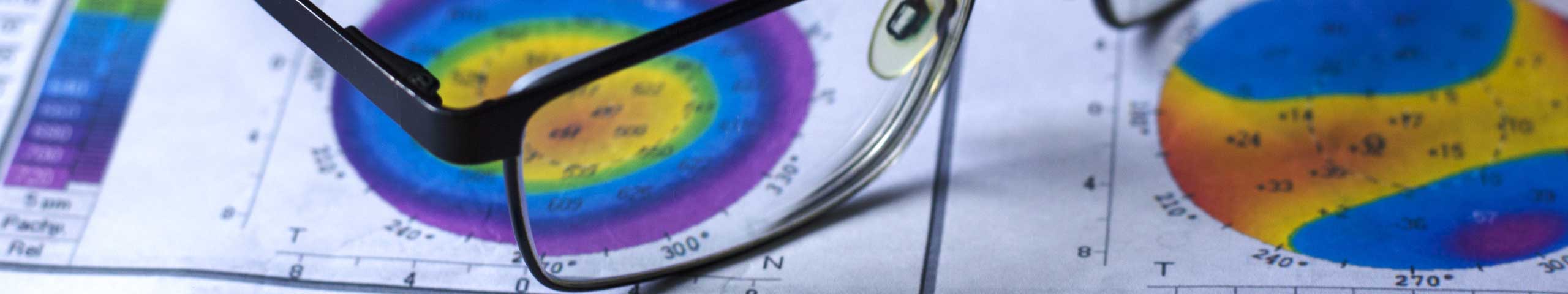
Meibomian gland dysfunction test
A comprehensive dry eye examination should include the following tests to thoroughly assess the degree of meibomian gland dysfunction:
- Ocular Surface Disease Index (OSDI) Questionnaire: fill out the questionnaire by clicking here.
- Blink frequency and quality
- Tear height measurement
- Tear osmolarity measurement (the salt content of the tears)
- Non-invasive tear evaporation test (how quickly the tears evaporate off the eye)
- Infrared Meibomian Gland imaging (shows the exact disease state of the meibomian glands within the eyelid) using the Oculus Keratograph
- Eyelid assessment by an optometrist or ophthalmologist
- Cell damage on the eye surface
Meibomian gand dysfunction treatment
Meibomian gland dysfunction treatment depends on the severity. It is tailored to each individual, based on contributing factors. It is important to remember that there is no quick fix for MGD, it requires on-going management. However just like brushing your teeth, treatment can become a simple part of daily routine.
Professional in-house treatments for MGD can be very effective, however results are maintained by continuing to do the at-home treatments.
A treatment plan for MGD usually consists of one or more of the following:
Diet Changes
The modern western diet has seen a significant shift from omega 3 oils (in oily fish, flax etc) to omega 6 (in seeds and vegetables). This shift is thought to have caused changes in how our bodies’ cells are made up. These changes have lead to a range of health problems. Increasing omega 3s in your diet, or taking an omega 3 supplement, can have anti-inflammatory properties and may help with MGD (2). Always talk to your GP about increasing the dose of omega-3s, as they thin the blood and increase the effect of some blood-thinning medications.
Eye Lid Hygiene
Bacteria live in the crust that forms on the bases of your eyelashes, so it is essential to effectively remove them. At The Eye Practice, we recommend using a proprietry product to effectively dissolve the crusts that build up along the edges of your eyelids.
We stock Blephadex and HypoChlor for home use. These products contain ingredients which kill the specific bacteria that cause blepharitis.
It is usual to use lid scrubs daily for several weeks to get the problem under control.
BlephEx
Just like our teeth need a professional clean every 6-12 months, so too do our eyelids. BlephEx is a fast, simple and relatively inexpensive in-house deep-clean treatment. It eliminates the build-up of bacteria and crusting that at-home cleaning leaves behind.
BlephEx can also be a great preparation for LipiFlow treatment.
Environment and glasses
Increasing humidity and improving work stations provides symptomatic relief from eye irritation and dryness. Simply wearing a pair of glasses increases the humidity around the eyes, thus helping relieve symptoms. The added benefit of prescription glasses is of course clear vision, reduced eye strain, and the latest spectacle lenses also help block the damaging blue light from digital devices from entering our eyes (read more about eye strain and blue light here).
Artificial tears
Sometimes eye drops can help with dry eyes, however it is important to avoid the drops that can make dry eye worse. An optometrist at The Eye Practice can recommend appropriate drops to use which will help with dry eyes rather than make them worse.
Optimel (Manuka Honey) Eye Gel
Manuka honey is a type of honey from bees that almost exclusively forage on the Manuka or tea tree plant in Australia and New Zealand. It contains anti-bacterial elements that seem to be effective against the bacteria that contribute to Dry Eye and meibomian gland dysfunction.
A recent study has shown that Optimel gel improves signs and symptoms of MGD significantly more when used in combination with warm compresses, compared to just using warm compresses alone (3).
It is important to use the gel form rather than the drop form, because the gel contains higher concentrations of the active ingredients and is preservative-free.
Prescription anti-inflammatory eye drops
Often, over-the-counter eye drops are not capable of reducing the inflammation that comes with moderate to severe Dry Eye and MGD. Usually these drops need to be compounded in order to be of the correct dosage and preservative-free.
Optometrists at The Eye Practice are therapeutically endorsed to write prescriptions for eye drops that can calm down the inflammation rapidly and improve Dry Eye symptoms dramatically.
Oral medications for meibomian gland dysfunction
Sometimes MGD requires a temporary course of oral antibiotics to improve symptoms. The antibiotics work to decrease the bacteria on the surface of the eye, and also improve meibomian gland oil quality. The traditional antibiotic used is called Doxycycline (4), however some recent research had shown that a different antibiotic called Azithromycin may be more effective (5).
Probiotics
In recent years there has been more and more evidence to suggest that our gut health can influence the health of our whole body, not just our digestion.
Probiotics are particularly helpful for people with facial and/or ocular rosacea, one of the causes of meibomian gland dysfunction.
The probiotic helps line the gut with healthy bacteria that reduce inflammation and skin flare ups – in turn reducing Dry Eye symptoms. It is important to find the right probiotic – many probiotics sold in pharmacies do not contain an adequate quantity of good bacteria.
Ultrabiotic products by BioCeuticals contain a high level of good bacteria. The bottles must be kept refrigerated, and it is recommended to take 2 capsules per day (e.g. 1 in the morning and 1 at night).
LipiFlow
LipiFlow unblocks meibomian glands, improves oil secretions and provides symptom relief. At The Eye Practice, all Dry Eye patients have a non-invasive assessment of their tear film oil level and oil glands to assess the chance of success with LipiFLow.
As LipiFlow is not a cure for MGD, it is important for patients to continue with their at-home treatments.
Intense Pulsed Light (IPL) Therapy
IPL is used for a variety of cosmetic skin conditions, including acne rosacea. It has also proven to be effective in improving meibomian gland secretions and treating MGD (6) (7).
It is quick and painless, and requires a series of at least 3 treatments to be most effective. Results are usually immediate and cumulative
For an assessment of your meibomian gland function and an effective, customised treatment plan, call us on (02) 9290 1899 or click here and make an appointment today.
References
- The international workshop on meibomian gland dysfunction: executive summary. Nichols KK, Foulks GN, Bron AJ, Glasgow BJ, Dogru M, Tsubota K, et al. s.l. : Invest Ophth Vis Sci, 2011, Vols. 52(4):1922-9.
- Topical omega-3 and omega-6 fatty acids for treatment of dry eye. Rashid S, Jin Y, Ecoiffier T, Barabino S, Schaumberg DA, Dana MR. s.l. : Archives of ophthalmology, 2008, Vols. 126(2):219-25.
- Randomised controlled trial of topical antibacterial Manuka (Leptospermum species) honey for evaporative dry eye due to meibomian gland dysfunction. Albietz JM, Schmid KL. s.l. : Clin Exp Optom, 2017.
- The international workshop on meibomian gland dysfunction: report of the subcommittee on management and treatment of meibomian gland dysfunction. Geerling G, Tauber J, Baudouin C, Goto E, Matsumoto Y, O’Brien T, et al. s.l. : Invest Ophth Vis Sci, 2011, Vols. 52(4):2050-64.
- Oral azithromycin versus doxycycline in meibomian gland dysfunction: a randomised double-masked open-label clinical trial. Kashkouli MB, Fazel AJ, Kiavash V, et al. s.l. : Br J Ophthalmol, 2015 Feb, Vols. 99(2):199-204.
- Prospective trial of intense pulsed light for the treatment of meibomian gland dysfunction. Craig JP, Chen YH, Turnbull PR. 2015, Investigative ophthalmology & visual science, pp. 56(3):1965-70.
- Prospective trial of intense pulsed light for the treatment of meibomian gland dysfunction. Craig JP, Chen YH, Turnbull PR. s.l. : Investigative ophthalmology & visual science, 2015, Vols. 56(3):1965-70.